Decompression Illness
To many people, the terms ‘decompression sickness’ (DCS), ‘decompression illness’ (DCI) and ‘the bends’ are synonymous. However, although there should be no difference in the immediate treatment of anyone suffering from these conditions, the terms do not necessarily mean the same.
Decompression Illness (DCI) is an umbrella term for both decompression sickness (DCS) and Cerebral Arterial Gas Embolism (CAGE).
Decompression Sickness
The “bends” is today readily associated with SCUBA diving. It is, in fact, an old-fashioned term used originally to describe the appearance of workers returning from ‘caissons’ during the construction of bridges in the 19th century. The air inside these underwater enclosures was pressurised (i.e. hyperbaric – greater than normal pressure) to counteract the weight of the surrounding water. Following their shifts, some men would return to the surface suffering joint pain that made it difficult for them to stand straight. Their appearance was similar to the ‘Grecian bend’ adopted by fashionable women of the time – hence the name. Many workers died or suffered permanent disability because of “Caisson disease”, as the condition became known. The connection between the workers’ return to the surface and their symptoms led to the introduction of surface based re-compression chambers to treat the afflicted. However, the reason for the condition was not fully recognised until 1878, when Paul Bert published his theory that the cause was the formation of nitrogen bubbles within the body. He also correctly stated that it was possible to avoid their harmful affects by ascending to the surface gradually – and that hyperbaric chambers worked, in part, because they decreased the size of bubbles.
Bert noted the work of the scientist Robert Boyle. In 1667, Boyle observed that following exposure to a compressed atmosphere, and subsequent decompression, a bubble formed in the eye of a viper. The animal also appeared distressed by the experience.
As stated by Boyle’s Law, ascending from a hyperbaric environment towards the surface results in an increase in the volume of a fixed amount of gas, including those found in the body. In the case of oxygen, the body quickly reabsorbs the extra volume as the cells use it up. Carbon dioxide, a waste product of metabolism, is excreted through the lungs very efficiently and therefore does not present a problem when decompressing.
The body does not use nitrogen, however, which forms almost 79% of the air. For the purposes of discussing decompression, it is an ‘inert’ gas. Unless enough time is allowed for it to be excreted through the lungs, any collection within the body’s tissues can increase in volume to the point where bubbles are formed. These can lead to the formation of emboli (singular: embolus) that cause adverse physiological effects by impeding blood flow, damaging tissues or nerves.
It should be noted that the presence of inert gas bubbles does not in itself lead to problems – what is important is the eventual size of these bubbles, their location, and the ability (or inability) of the body to rid itself of them before they cause damage.
For further information on decompression theory, please refer to the dive tables section. Gas diffusion (Dalton’s law) and Boyle’s law are discussed in the principles section.
Classification of Decompression Sickness
In addition to the “bends”, the effects of “Caisson disease” have several other descriptive terms. The “chokes”, “staggers” and “niggles”. These are discussed below.
The label ‘decompression sickness’ (DCS) was introduced in place of “Caisson disease”. Decompression sickness can be classified as either Type 1 or Type 2. The different classification reflects the effect, and therefore the severity, of the condition. Diagnosing DCS as one (or both) of just two categories does not enable proper identification or discrimination. However, for the sake of completeness, the two types are described here.
Type 1 DCS can occur when bubbles affect the tissues around skeletal joints. Symptoms usually include unilateral (on one side of the body) discomfort or pain in one or more joints. The areas most often affected are the knees, elbows and shoulders.
Decompression sickness might also present as a skin (cutaneous) disorder. Nitrogen bubbles can cause mottling, lumps or a rash. “Skin bends”, as they are colloquially termed, are more common during hyperbaric chamber ‘dives’ and when diving using a dry suit. Although not usually in themselves serious, skin symptoms may indicate the presence of problems elsewhere. A particularly serious cutaneous sign of DCS is ‘cutis marmorata’ marbling, in which an area of skin becomes pale with dark mottling. This is associated with considerable development of inert gas bubbles within the body.
If left untreated, Type 1 DCS may progress to Type 2.
Type 2 decompression sickness reflects involvement of the Central Nervous System (CNS) and / or the cardio-respiratory system. More than half of those diagnosed with DCS will be classified as Type 2.Cerebral symptoms arise from interruption of the blood supply to the main part of the brain, and include confusion, reduced mental function and unconsciousness. Involvement of the cerebellum may lead to tremors, loss of balance (“staggers”) and a lack of co-ordination (ataxia). Balance may also be affected by damage to the vestibular part of the inner ear.
Spinal DCS may present as back pain, paresthesia (pins and needles), paralysis and loss of urinary sphincter control – resulting in either incontinence or retention.
As discussed already, the formation of small inert gas bubbles does not necessarily lead to the development of DCS. Likewise, when bubbles become trapped in the tiny blood vessels around the lungs’ alveoli (air sacs), problems do not always arise. In fact, it is thought that their accumulation in this area may increase the rate that the gas is excreted from the body (Edmonds et al, 1993). However, if too many bubbles collect, breathing will become adversely affected (“chokes”). Symptoms include breathlessness, tachypnoea (increase in breathing rate), chest pain and coughing. Although symptoms may resolve, this should be regarded as a life-threatening condition as it may progress to fatal respiratory collapse.
Signs and Symptoms of Decompression Sickness
A more useful classification of DCS can be achieved by noting the area(s) of the body affected. These are detailed in the following list.
General signs (constitutional).
- Nausea, weakness or fatigue.
Skin (cutaneous).
- Itching (pruritis).
- Generalised rash.
- Lumps.
- Cutis marmorata marbling (serious sign).
- Crackling feeling (subcutaneous emphysema) – not usually around collarbone.
Musculoskeletal (muscles and joints).
- Joint or muscle discomfort and / or pain (“bends”).
- Limitation of limb movement.
- Crunching sound in joint.
Gastrointestinal (stomach and bowel).
- Nausea, vomiting.
- Abdominal cramps, diarrhoea.
Cardiorespiratory (heart and lungs).
- Coughing.
- Chest pain made worse on inspiration.
- Tachypnoea (increase in breathing rate).
Neurological (cerebrum, cerebellum, spinal cord, inner ear and peripheral nerves).
- Headache.
- Confusion.
- Memory loss.
- Tremors.
- Visual disturbance (scotoma).
- Involuntary eye movement (nystagmus).
- Lack of co-ordination (ataxia).
- Numbness or altered sensation.
- Pins and needles (paresthesia).
- Urinary retention.
- Ringing sound in ears (tinnitus).
- Hearing loss.
- Dizziness, loss of balance (vertigo).
- Partial or full paralysis of lower limbs (paraparesis / paraplegia).
- Unconsciousness.
It must be emphasised that even in the absence of obvious symptoms, the possibility of DCS should be considered if the diver’s circumstances suggest such a risk. If in any doubt, contact the appropriate service – see the contact section.
Those with any symptoms of DCS, however mild, are at risk of further episodes.
Cerebral Arterial Gas Embolism
The term is self-explanatory; gas (air) forms an embolism (blockage) in an artery (vessel supplying blood) in the cerebrum (brain). This is caused by rupture of the fragile lining of the lung’s alveoli allowing large quantities of air to enter the blood vessels leading to the small arteries in the brain via the heart.
CAGE is a life-threatening emergency and requires immediate medical treatment.
Signs and symptoms of CAGE
Cerebral Arterial Gas Embolism is the result of pulmonary barotrauma, which may present with the following symptoms.
- Subcutaneous emphysema, particularly around collarbone area.
- Chest pain.
- Shortness of breath (dyspnoea).
- Coughing, possibly with blood (haemoptysis).
- Increase in heart rate (tachycardia).
- Decrease in blood pressure (hypotension).
The resulting cerebral damage may result in the following symptoms.
- Severe headache.
- Paralysis.
- Numbness.
- Unconciousness.
Symptoms similar to those of neurological DCS may also be present. Any confusion between the diagnosis of CAGE or neurological DCS should not influence the immediate care of the affected diver – both are medical emergencies treated initially in the same way.
Predisposing Factors
The risk of developing decompression sickness depends on many factors, most of which are not yet clearly understood. Some of these are discussed below – click on a link or scroll down the page.
| PFO | Flying | Exercise | Smoking | Alcohol |
| Obesity | Repeated Dives | Temperature | Breathing Gas | Age & Gende |
Patent Foramen Ovale (PFO)
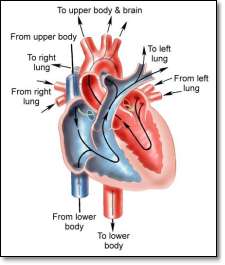
One of the most significant predisposing risk factors in DCS is a physical abnormality of the heart called Patent Foramen Ovale (PFO) – a small opening between the upper two chambers of the heart (atria).
Every unborn baby has a Foramen Ovale that allows blood already oxygenated by the mother’s lungs to by-pass the baby’s respiratory system. The opening usually seals up following birth. If it remains open (patent) then it can cause a ‘short circuit’ of blood flow allowing bubbles to pass directly from the venous circulation to the brain through the heart, bypassing the filtering effect of the respiratory system. The diagram on the right shows normal blood flow around the heart (black arrows) and the route of blood and bubbles through a PFO (green arrow). Click on the diagram for a larger view.
A more severe form of this abnormality is Atrial Septal Defect (ASD), which is likely to have already been diagnosed since the signs and symptoms are more obvious – usually from an early age. The symptoms include heart murmur, cyanosis and faintness.
PFO is present in about 25% of the general population and does not normally cause health problems. However, it affects up to 75% of divers with ‘unexplained’ DCS (Kerut et al, 2001). Although PFO increases the risk of decompression sickness, individuals with PFO do not necessarily develop symptoms. Also, even in the absence of any apparent cause, DCS is not always due to a PFO.
Because most people with PFO show no obvious signs, diagnosis is usually only attempted following an unexplained incidence of DCS. Closure of the defect is possible using surgery, but the benefit of undergoing such a procedure should be balanced against the risks involved. Those who have suffered a significant episode of DCS are more susceptible to it in the future if they continue to dive, whether or not the PFO is repaired.
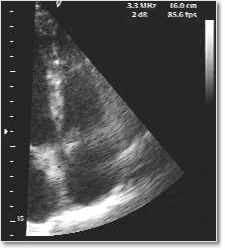 The test to confirm PFO uses an echocardiograph machine to indicate the presence of blood flow between the two atria of the heart. A cardiologist, following referral by a specialist in hyperbaric medicine, normally carries out testing.
The test to confirm PFO uses an echocardiograph machine to indicate the presence of blood flow between the two atria of the heart. A cardiologist, following referral by a specialist in hyperbaric medicine, normally carries out testing.
Several types of tests are possible. One of the most common is a trans-thoracic echocardiogram (TTE). In this procedure, an ultrasonic probe similar to one used for foetal ultrasound scans, is passed over the patient’s chest – giving a visual representation of the four chambers of the heart on a VDU screen. A special solution of saline called a contrast medium is infused quickly into the venous circulation.
This results in a sudden flow of small gas bubbles to pass through the right side of the heart – first the right atrium and then immediately after, the right ventricle. If a PFO is present, the bubbles will also be seen passing from the right atrium to the left one. The image on the right is taken from a recording of a TTE test. The four chambers of the heart can be clearly seen (the atria are at the bottom of the picture).
Flying after Diving
As discussed in the principles section, surface atmospheric pressure is a result of the air above us. Because there are fewer molecules of gas at higher altitude, there is less pressure and therefore a lower partial pressure of each gas in the air – which means there is less oxygen available. This hypobaric effect is the opposite of hyperbaric pressure.
This concept is familiar to most people since aircraft flying at high altitudes must have pressurised cabins to support life. All commercial passengers are reminded that in the event of sudden cabin de-compression oxygen masks will drop down from above. However, in normal operation, the cabin ‘altitude’ can be as high as 7,500 – 8,000 feet.
Although reducing the available amount of oxygen to the body can lead to hypoxic conditions, most healthy people will not experience symptoms during a normal commercial flight. The main risk to divers from flying is not the reduction in oxygen partial pressure, but the reduction in atmospheric pressure itself.
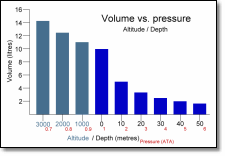
As can be seen on the graph to the right, as pressure decreases with increasing altitude, the volume of a gas will increase. Although the degree of change in a hypobaric atmosphere is less pronounced than in a hyperbaric atmosphere, pre-existing nitrogen bubbles in the body will grow larger and may exacerbate or even cause DCS. Larger gas spaces, such as a pneumothorax, will also grow.
The length of time required between a dive and flying depends on many factors, e.g. depth, duration and number of dives, therefore it is impossible to give a definitive pre-flying period. However, it is recommended that following SCUBA diving an individual should wait 12 to 24 hours before flying (Divers Alert Network). Before flying, it is worth considering several points:
- Everyone undergoing de-compression from a hyperbaric air atmosphere will accumulate nitrogen that will tend to form bubbles.
- The more time the body has to excrete nitrogen, the less likely bends are.
- Commercial aircraft cabins are only pressurised to about 0.8ata (7,500 feet).
- Failure of cabin pressure at altitude may result in severe decompression illness in those already carrying excess nitrogen.
- Medical resources for the treatment of DCI are limited on passenger aircraft.
 Exercise
Fit, healthy individuals are less likely to suffer from most medical conditions than unfit ones but there are possible risks involved with strenuous physical exercise.
It has been suggested that strenuous exercise causes the formation in the body of tiny gas bubbles called ‘micronuclei’ (Dervay et al, 2002). It takes several hours for these bubbles to disperse and although no absolute link has been established between the existence of micronuclei and decompression illness, it is recommended that strenuous exercise be avoided for four hours before SCUBA diving (Divers Alert Network).
There is, however, contradictory research into exercise around the time of diving (Wisloff and Brubakk, 2001; Jankowski et al, 1997). Moderate exercise is known to improve blood circulation in muscle tissue and increases cardiopulmonary function therefore may help to increase the rate of nitrogen excretion from the body.
Physical exercise is most beneficial when done in moderation as part of a healthy lifestyle. Avoiding strenuous exercise may be difficult to avoid but seems to be a worthwhile precaution.
Smoking
Considering the importance of effective respiratory function, the effects of smoking can have a considerable affect when SCUBA diving.
Cigarette smoke contains carbon monoxide (CO), which is a poison. The amount of CO in a smoker’s body can be as high as 10%, compared to less than 2% for a non-smoker. This increased level reduces the ability of the red blood cells to carry oxygen. Cigarette smoke also contains nicotine, which acts as a vasoconstrictor and may theoretically increase the risk of DCS due to altered blood perfusion.
Longer-term problems include chronic obstructive pulmonary disease (COPD) which leads to reduced oxygen availability and an increase in carbon dioxide (CO2) retention in the body. This has been implicated as a factor in CNS oxygen toxicity. Smokers are also generally less healthy and are more prone to develop circulatory problems. Refer to the CO poisoning section for further details on the effects of carbon monoxide.
Alcohol
The effects of alcohol on co-ordination, consciousness and mental reasoning are well documented and have obvious implications in the ability of a diver to carry out the tasks necessary for a safe dive. This reduction in ability also applies to a ‘hangover’.
Alcohol will increase the chances of developing nitrogen narcosis due to the depressant effect on the central nervous system. As with any CNS condition, intoxication following a dive will potentially mask some of the symptoms.
Alcohol is also a powerful diuretic that will increase urine output and promote dehydration during diving – one of the risk factors in DCS.
Obesity
An increase in adipose (fat) tissue leads to an increase in nitrogen loading in the body, since nitrogen is five times more soluble in fat tissue than muscle. Because fat can absorb more gas than muscle, it will take longer for the body to excrete it. It is assumed that there is a greater risk of decompression sickness.
Obesity also increases the body’s oxygen requirements, leading to a likely reduction in physical ability. The long-term implications of obesity are well known. Conditions related to obesity such as diabetes and coronary artery disease are themselves risk factors.
Repeated Dives
Following each dive the body retains some of the inert gas dissolved in the tissues. The correct use of dive tables usually allows enough of the gas to be excreted via the lungs to avoid the formation of bubbles large enough to cause physiological problems. Repeated dives will increase the risk of DCS if adequate time is not allowed to offload the dissolved gas. For the same reason, the depth and duration of the dive will influence the amount of absorbed gas.
Temperature
SCUBA diving in warm water will generally result in higher nitrogen loading than in cold water. This is due mostly to the effects of vasodilatation.
The general effects of cold on the body are discussed further in the hypothermia section.
Breathing Gas
Certain alternatives to standard air can be used for SCUBA diving. The unique properties of each gas, and mixture, should be fully considered to determine a safe dive profile.
Age and Gender
There are conflicting studies showing the existence, or lack, of a relationship between a diver’s age / gender and the incidence of decompression sickness. A study by the Armstrong Laboratory concluded that there is a three-fold increase in high altitude DCS in men over 42 years old compared to those aged 18-21. The reason for any increased risk in dive related DCS might be due to the distribution and amount of fat in the diver’s body.